Briana Gallinari, NTI Phlebotomy graduate, Scarborough campus.
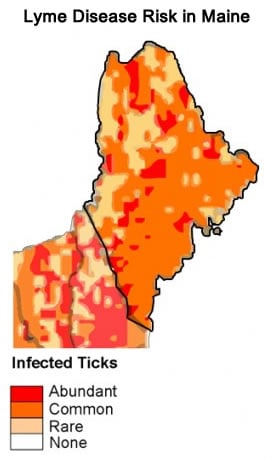
What the heck is that? Do you mean the fruit? Doesn’t that come from tropical islands? And inquisitive looks, are just a few of the many hilarious responses I encounter when I mention that I have Lyme Disease (LD). I’d like to begin with a few misconceptions. It’s just Lyme disease, not Lymes disease. Now back to that tropical islands comment. LD is not confined to warmer climates, in fact, Antarctica is the only continent LD hasn’t spread to. Although ticks don’t migrate, birds do, and ticks can feed off of any mammal. Small ones that live in our yards, such as birds, squirrels, chipmunks, and rabbits are among their favorite targets. These cute critters often bring more ticks into our yards, putting us at higher risk of getting bit. Many people with LD have (reluctantly) opted to remove their bird feeders in order to reduce their risk of becoming re-infected.
Let’s jump back to misconceptions for a minute. Many people believe that a tick must be attached for a certain length of time in order for a person to contract LD. This is untrue, the moment a tick is attached it begins sucking and regurgitating, it takes less than a minute to become infected. Another common misconception is that ticks or a certain species of ticks are the only transmitters of LD, or that LD is the only infection they can transmit. Ticks and many other bugs including but not limited to spiders, fleas, lice, and mosquitos (really anything that bites) have the potential to transmit LD and many other infections known as co-infections. Common co-infections include Rocky Mountain Spotted Fever, Babesia, Cat Scratch Fever, Bartonella, Ehrlichiosis, and many more. Co-infections are not the only thing that could accompany LD through a bite either. Many viruses, parasites and other pathogens can be transmitted as well.
 A handful of people have confidently told me that they could never get bit by a tick because they would feel it crawling on them. It’s nice in theory, that you would notice teeny little legs tickling your skin as it searches for the warmest spot to hunker down for a meal. And perhaps they always say it so confidently because they’ve only seen ticks in photos, or full grown adult ticks that are freckle sized. May was deemed Lyme Disease Awareness Month for a very good reason, this is the time of year when they are re-emerging from the cold winter months. So why don’t I see them? You may be wondering. Excellent question! During this season the nymphs, or baby ticks, are most prevalent. Those suckers are smaller than the period at the end of this sentence. Don’t be fooled by their size though, they carry just as much disease as an adult tick does, they are just much MUCH harder to spot.
A handful of people have confidently told me that they could never get bit by a tick because they would feel it crawling on them. It’s nice in theory, that you would notice teeny little legs tickling your skin as it searches for the warmest spot to hunker down for a meal. And perhaps they always say it so confidently because they’ve only seen ticks in photos, or full grown adult ticks that are freckle sized. May was deemed Lyme Disease Awareness Month for a very good reason, this is the time of year when they are re-emerging from the cold winter months. So why don’t I see them? You may be wondering. Excellent question! During this season the nymphs, or baby ticks, are most prevalent. Those suckers are smaller than the period at the end of this sentence. Don’t be fooled by their size though, they carry just as much disease as an adult tick does, they are just much MUCH harder to spot.
The most important thing to remember if you do get bit, is proper removal. Many tricks such as smothering it so it backs out on its own, burning, or squeezing it can be very dangerous as it can cause the tick to regurgitate while it’s still attached. The goal is to not squish its body in the process of removal, and to ensure complete removal. It’s very easy for the head of the tick to remain attached to the skin after the body has been pulled away. If you consider yourself gifted with dexterity you can carefully use a pair of tweezers to grasp the tick at the base where it’s attached to the skin and use a twisting motion to pull it off. If you can remove it with skin still in its mouth, you may rejoice as you’ve just succeeded in proper tick removal! If that sounds a little too nerve wracking, there is actually a handy little tool shaped like a teaspoon with a “V” shape cut into one end so you can scoop the tick right into the tool from your (or your pets) skin. It’s called TICKED OFF and costs about $4. However if the tick is very small and hard to see, it’s best to call your doctor to have it removed immediately. I know it sounds silly to go to your doctor for something you’ve probably done a million times. But it’s better to be safe than sorry. My mom brought me in for a tick removal once when I was very young and my doctor actually laughed at her when she called to say why she needed to bring me in. After examining the tick (with magnifying glasses I might add) she told my mom she did the right thing bringing me in, and even sent the tick for testing and sent my mom and I home with a list of symptoms to look out for. Thankfully that was not the tick that infected me.
Most people infected with Lyme disease never see the tick that bit them. And only about half see the bull’s-eye rash (in case you’re wondering, that rash is only associated with LD and nothing else). The bull’s-eye rash is a red expanding ring that looks much like a target, hence its name. The rash will normally clear up all on its own relatively quickly, and is no indication as to whether or not the patient is getting better. Some of the most common symptoms of LD include headaches, brain fog, speech problems, hearing problems, vision problems, insomnia, fatigue, light sensitivity, noise sensitivity, dizziness, confusion, disorientation, anxiety, mood disorders, fainting, irregular heartbeat, chest pain, fever, cough, difficulty breathing, weight gain or loss, stroke, abdominal pain, nausea, vomiting, bladder pain, thyroid dysfunction, inflammation in the body, allergies, unexplained sweats, joint pain, joint swelling, arthritis, muscle pain, muscle spasms, muscle cramps, muscle weakness, tingling, numbness, and difficulty walking. Due to the wide range of symptoms, LD is known as “The Great Imitator” as it mimics so many other diseases and illnesses. This leads many patients to be misdiagnosed for years before someone finally sees the true cause of their symptoms. I was very fortunate that it only took me six months to get diagnosed. Unfortunately, treatment in children is complex and not fully understood, which meant that my doctors didn’t really know how to treat my illness. Because I wasn’t treated correctly I progressed from Acute LD to Chronic LD. For years physicians fought over whether or not chronic Lyme disease even existed, though recently they discovered that it does exist, and that it needs its own form of treatment. Even today physicians still can’t agree on safe forms of treatment for either stage, which leaves many patients floundering.
Personally, I’ve traveled all over the U.S. for treatment. In the process, I’ve met wonderful people who have also traveled all over the U.S. and even outside the country for treatment. Most of my friends these days are fellow sick people, whether they have LD or not. We share advice, support, information, and above all else we can relate to one another. When I got sick at 15, most of my friends at the time didn’t really know how to continue being my friend when I was suddenly bed-bound. So, most of my relationships came to an awkward end in the middle of high school. As I traveled for treatment and spoke more about LD, connections just started forming, and it just so happened to be with other people who in some way, had “been there”. We had all walked different paths but with the same busted shoes (bad shoes/body metaphor?). We had a type of understanding that simply can’t be put into words. Some, people with LD even refer to themselves and their LD buddies as Lymies. There are many forums and online communities for Lymies to share support and information as well, which is one of the best resources a Lymie could have. There is a lot of information that can only be accessed by patients sharing their experiences. For instance, some of the best physicians I’ve seen, I never would have known about if it hadn’t been for another patient’s recommendation.